Efficient Techniques for Recovering Irritable Bowel Syndrome (IBS).
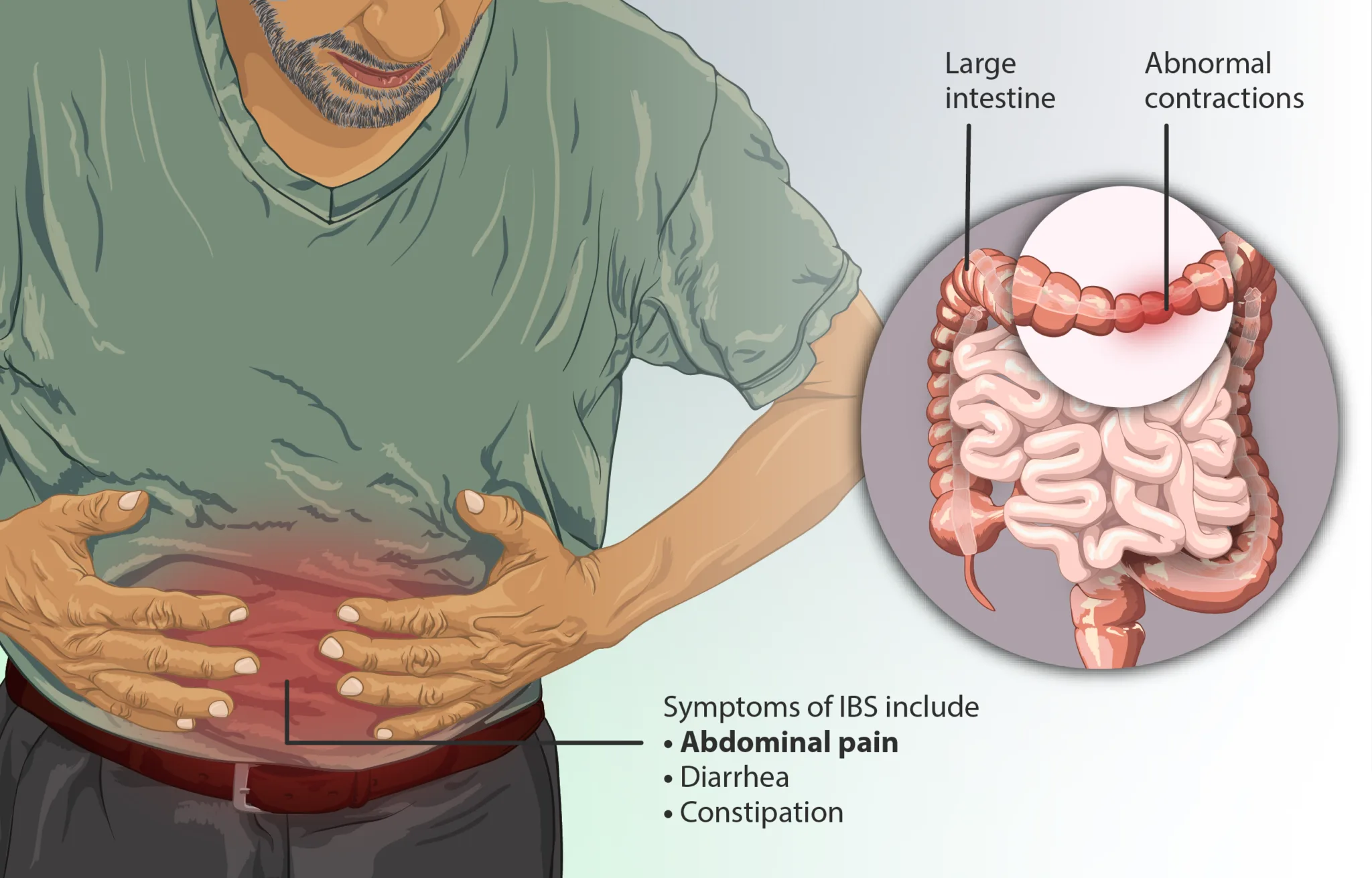
Irritable Bowel Syndrome (IBS) is a common digestion disorder that affects countless people worldwide, characterized by symptoms such as bloating, stomach pain, constipation, diarrhea, and irregular defecation. Regardless of being a prevalent condition, the precise reasons for IBS stay elusive, making it a complex syndrome to manage. This condition, which is typically chronic, can disrupt the life of those impacted, as it hinders digestion and causes significant pain. While lots of seek conventional treatments like medication or dietary changes, a growing variety of people are turning to origin techniques to recover IBS from within, focusing on long-term services instead of sign management alone.
At the core of handling IBS successfully is understanding that it is not just a gastrointestinal problem. Instead, it frequently comes from a mix of aspects such as gut dysbiosis, tension, food level of sensitivities, and way of life routines. A root cause approach involves identifying these underlying factors and addressing them directly, allowing for more lasting relief and healing.
Gut Health and IBS.
The health of the gut microbiome is intricately linked to IBS. Our gut is home to trillions of bacteria, many of which are essential for digestion, nutrient absorption, and overall immune function. Nevertheless, an imbalance in these germs, typically described as "gut dysbiosis," can add to the beginning and progression of IBS symptoms. Restoring balance in the gut is, therefore, among the primary steps towards recovery the disorder.
One way to begin this process is by including probiotics and prebiotics into the diet plan. Probiotics are useful germs that can help restore balance in the gut microbiome, while prebiotics act as food for these germs, helping them grow. Lots of people with IBS have reported improvements in their symptoms after regularly taking probiotics and guaranteeing their diet supports gut health. Foods rich in probiotics consist of yogurt, kefir, and fermented veggies like sauerkraut. Prebiotic-rich foods include bananas, garlic, onions, and asparagus.
In addition to probiotics, dietary changes can substantially affect gut health. An elimination diet, which includes eliminating potential trigger foods and slowly reestablishing them, can help recognize particular food sensitivities or intolerances that might be contributing to IBS signs. Common triggers for those with IBS include gluten, dairy, and particular types of carbohydrates called FODMAPs. A low-FODMAP diet, which includes minimizing foods high in fermentable carbohydrates, has actually been commonly recognized as a reliable dietary technique for managing IBS.
Tension and the Gut-Brain Connection.
The gut-brain axis is a bidirectional communication system between the gut and the brain. This connection plays a significant function in the manifestation of IBS signs. Stress and stress and anxiety can intensify IBS, leading to flare-ups and getting worse gastrointestinal issues. The nerve system, particularly the vagus nerve, straight influences gut motility and level of sensitivity. Therefore, resolving stress is vital when it comes to handling and healing IBS.
Mind-body practices such as mindfulness meditation, yoga, and deep breathing workouts have revealed promise in minimizing the severity of IBS symptoms by relaxing the nervous system. These practices can help in reducing stress, promote relaxation, and enhance gut function over time. Regular exercise also contributes in reducing stress levels and promoting healthy food digestion.
Incorporating tension management strategies into daily life can have extensive effects on gut health and general wellness. For example, cognitive-behavioral therapy (CBT), a kind of IBS psychotherapy, has been utilized successfully in individuals with IBS to help them manage tension and develop coping systems for their signs. This approach highlights the significance of resolving not just the physical aspects of IBS however likewise the psychological and emotional elements.
Hormone Influence on IBS.
For some individuals, hormone imbalances can contribute in triggering or aggravating IBS signs. Females, in particular, may discover modifications in their digestion health around their menstruation. Fluctuations in estrogen and progesterone can affect gut motility, resulting in either irregularity or diarrhea. Throughout certain times of the menstrual cycle, IBS symptoms may become more noticable, specifically in those who are currently inclined to the condition.
Addressing hormonal imbalances through natural techniques such as dietary changes, herbal supplements, and way of life modifications can assist alleviate their influence on IBS. For example, balancing blood sugar levels, improving sleep quality, and reducing inflammatory foods from the diet can contribute to better hormonal regulation. Herbal supplements like chasteberry or evening primrose oil may also help support hormonal balance, though it's important to consult with a healthcare provider before starting any supplementation.
Inflammation and IBS.
Chronic swelling in the gut can be another key factor to IBS signs. Swelling can harm the lining of the gut, causing increased intestinal tract permeability, typically described as "leaking gut." When the gut lining is compromised, toxic substances and undigested food particles can go through the digestive tract wall, triggering an immune response that causes more swelling and gastrointestinal distress.
Healing the gut lining is an important part of dealing with IBS at its root. Nutrients like L-glutamine, an amino acid that supports the repair of the gut lining, can be helpful for those with IBS. In addition, integrating anti-inflammatory foods into the diet, such as turmeric, ginger, and omega-3 fatty acids, can help in reducing inflammation and promote gut healing.
Reducing swelling through lifestyle changes is likewise essential. Chronic stress, bad sleep, and an inactive lifestyle can all add to increased swelling in the body. By adopting a more well balanced way of life, individuals with IBS can help alleviate the results of inflammation and enhance their total gastrointestinal health.
A Personalized Approach to Healing IBS.
One of the obstacles of treating IBS is that there is no one-size-fits-all option. Every individual with IBS might have different triggers, signs, and underlying causes. Therefore, a personalized technique to recovery IBS is crucial. Dealing with a healthcare expert or a practical medicine practitioner can assist identify particular elements adding to IBS and create a personalized treatment plan.
This plan might consist of a combination of dietary modifications, stress management methods, gut-healing protocols, and supplements. By addressing the origin of IBS, individuals can work towards long-term relief instead of just handling symptoms.
Furthermore, testing for food level of sensitivities, hormone levels, and gut health markers can supply valuable insights into the particular areas that need attention. For instance, testing for small digestive bacterial overgrowth (SIBO) can help determine whether an overgrowth of germs in the small intestine is contributing to IBS signs. Addressing SIBO with targeted treatment, such as prescription antibiotics or herbal antimicrobials, can lead to considerable enhancements in gut health.
Conclusion.
Healing Irritable Bowel Syndrome (IBS) needs a holistic approach that exceeds simply treating symptoms. By concentrating on the root causes of the disorder, such as gut dysbiosis, tension, hormonal imbalances, and inflammation, individuals can attain long-term relief and improved gastrointestinal health. While the journey to recovery may take some time and effort, resolving these underlying factors through dietary changes, tension management, and personalized care can cause lasting improvements. Dealing with health care professionals to tailor a plan that fits your special needs can make all the difference in managing IBS efficiently. Through a dedication to lifestyle changes and understanding the intricacy of the gut-brain connection, it is possible to gain back control over your digestive health and lead a more comfortable, symptom-free life.